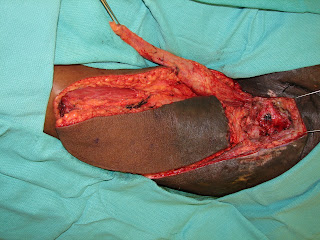
Long standing burn scars can have tumors arise in them called Marjolin's Ulcers. It is important to excise these ulcers with wide surgical margins.
Often the resulting defect that occurs can not be closed primarily and tissue needs to be borrowed from one region of the body and transferred into the defect. The axillary flap can be easily rotated into close defects on the anterior chest.
This flap allows for a better contour of the chest wall skin withou a visible or palpable depression that may occur with a skin graft.
Once the anterior chest wall wound is closed, drains are placed to evacuate any fluid from beneath the wound to prevent infection.
Post-operatively, the flap allows for adequate contour of the chest and for a closed wound.
It is not uncommon for many patients to have a wound or lesion present on their body for quite sometime. Often as these lesions are wounds grow larger, it becomes more difficult to excise, clean, or close these wounds.
What it is important for patients to know, is that there is always a solution or help that they can receive from Plastic & Reconstructive surgeons to make the wound cleaner, more manageable, or possibly close with a flap.
While the reconstructive process can often take time, patients are always happier with a closed wound that they no longer need to take care of.
http://www.drbriandickinson.com/